Joint Assets: An Osteoarthritis Update

The aching, swollen, stiff joints associated with osteoarthritis (OA) have long been considered a “wear and tear” condition, associated with aging. It was thought that cartilage, the smooth connective tissue on the end of bones that cushion the joints, simply breaks down over a lifetime of walking, exercising and moving. New research shows that it is a disease of the entire joint that also causes bony changes of the joints, deterioration of tendons and ligaments and inflammation of the synovium (lining of the joint). While more prevalent in people over 50, OA can show up in younger patients, especially those who’ve experienced a joint injury such as a torn ACL or meniscus. The promising news is that according to the Arthritis Foundation, “OA is not an inevitable aging disease” and the Cleveland Clinic notes: “Age is a contributing factor, although not all older adults develop osteoarthritis and for those who do, not all develop associated pain.”
Still, currently OA is by far the most prevalent form of arthritis, affecting more than 32.5 million Americans, and primarily targeting knees, hips, hands and spine. A variety of factors contribute to the development of OA, including congenital joint deformity, family history, previous joint injury, and years of physically demanding work or contact sports. However, reducing risk is possible with attention to these modifiable factors:
- Obesity adds stress and pressure to joints. Consider that your knees bear a force equivalent to three to six times your body weight with each step, so a lighter weight relieves the burden considerably – losing one pound takes 3 pounds off the knees.
- Lifestyle. Being physically active is crucial, as a sedentary lifestyle and obesity are associated with a higher risk of OA. While sports such as football, baseball and soccer may pose a risk because of their impact on joints, most types of regular or moderate exercise can be safely done.
Living with Osteoarthritis
Unfortunately, there is no cure for OA, and managing symptoms such as joint stiffness, tenderness, swelling, and popping or crackling can become increasingly difficult over time. While seeking a pill to alleviate discomfort is a natural reaction, consider trying alternative solutions to help break the cycle of chronic pain.
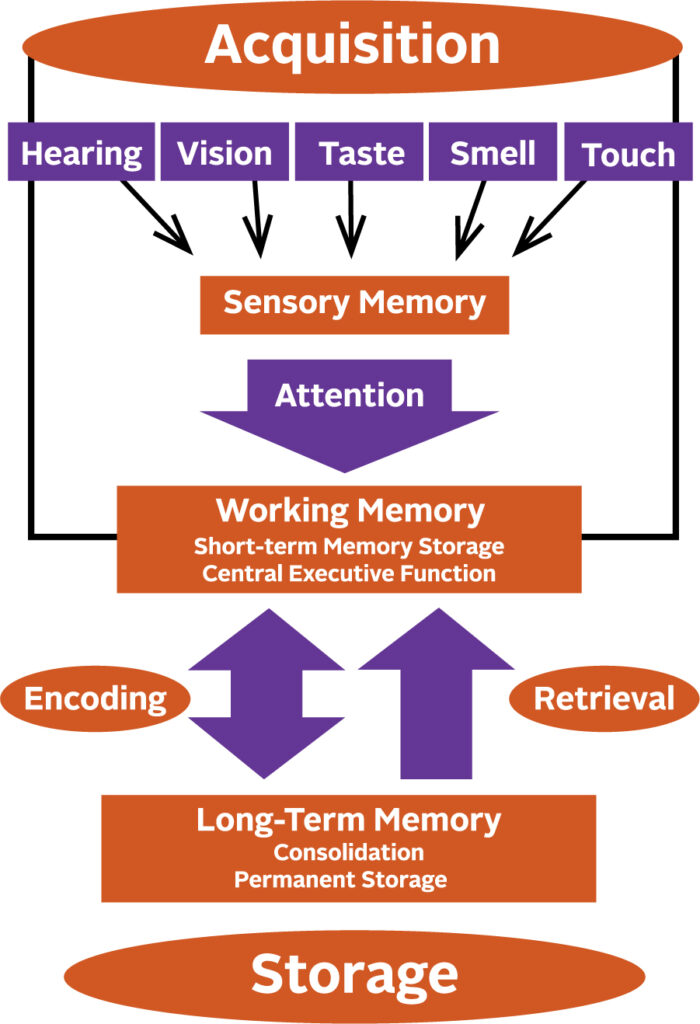
“The longer the brain processes pain, the more hypersensitive it becomes to pain,” explains Rachel Welbel, MD, a physiatrist who is extensively trained in physical medicine and rehabilitation and sports medicine. “The brain, now constantly on high alert, may respond to non-painful sensations as if they are painful. Poor diets and stress can increase chemicals in the brain that reinforce this response, prolonging the pain cycle.”
Reflecting a more holistic and multi-faceted approach to managing pain, she says: “Opioids are almost never the answer.” Instead, she recommends lifestyle modifications, treatments and medications that help tackle pain in a variety of ways.
Lifestyle Modifications, Treatments and Medications for Osteoarthritis
Weight management. Obesity is not only a leading risk factor for OA, but adds to the pain for those with the condition. Body fat produces proteins called cytokines that cause inflammation, and in the joints, can alter the function of cartilage cells. Shedding even a few pounds can make a difference: losing just 10% of your body weight can cut arthritis pain in half, and losing another 20% can reduce the pain by an additional 25% or more, and may slow or even halt progression of the disease.
Exercise and movement. “Exercise is key to living well with OA,” says Welbel. “While resting aching joints may bring temporary relief, lack of movement ultimately leads to more discomfort. The focus is not on weight loss but on minimizing pain and maximizing strength.” Plan on 150 minutes of light to moderate exercise each week. She recommends working with a physical therapist who can analyze your joint biomechanics and suggest exercises to strengthen muscles and improve range of motion while reducing stiffness and pain. “In addition, exercise is a natural mood elevator,” says Welbel. “Walk, swim, or try mindfulness-based, stress-reducing exercise such as yoga and tai chi.”
Anti-inflammatory diet. Increasing consumption of fruits, vegetables, whole grains, legumes and fish, while reducing consumption of red and processed meats, refined grains, and sugar-containing beverages and foods, may play an important role in reducing pain associated with inflammation from OA, says Welbel. Try incorporating into your diet fatty fish; herbs and spices such as garlic, turmeric and cinnamon; yogurt and other fermented foods; and healthy fats such as avocados, extra virgin olive oil and walnuts.
Supportive devices. A cane or walker can help lighten the load on your joints, decrease pain, and reduce your risk of falling. Intermittent use of a knee brace may be helpful for added stability, especially if walking on uneven surfaces. Foot orthotics such as arch supports and metatarsal pads may reduce foot pain.
Medications. Over-the-counter (OTC) pain relievers like acetaminophen (Tylenol) may help joint pain and stiffness for some. Nonsteroidal anti-inflammatory drugs (NSAIDs) are also used to relieve pain, including OTC medications such as Advil or Aleve, or Celebrex, a prescription medication with a somewhat lower risk of ulcers and upper gastrointestinal bleeding than other NSAIDs. Topical NSAIDS such as Aspercreme and other creams or patches containing ingredients such as capsaicin, menthol or lidocaine can help.
Injections. Corticosteroids injections may provide temporary relief for acute flare-up of OA pain in knees and finger joints, but effectiveness can vary, and you must wait at least 3 to 6 months to repeat an injection in a specific joint if needed. Viscosupplementation involves injection of a gel-like substance containing hyaluronic acid, which acts as a lubricant in the fluid between bony surfaces and is decreased in OA joints. Research results for significant pain reduction or improved function are not yet convincing, but there appear to be a number of patients with mild to moderate knee OA who report symptom relief.
Supplements. Research results are mixed, but we note some of the more well-known supplements with the caution that these are not recommended to be used alone as treatments for OA. Glucosamine and chondroitin sulfate, naturally occurring compounds found in healthy cartilage, may help reduce joint pain and stiffness, and have been available in the U.S. and Europe for several decades. Other supplements such as tart cherry and turmeric may help reduce OA symptoms for some.
Other promising but not yet proven treatments. Platelet-rich plasma (PRP) injections and stem cell therapy have been used to treat pain of mild to moderate knee OA, but evidence of effectiveness is mixed, and these are still considered experimental. Elements of Eastern medicine, including herbs and acupuncture, may help control OA symptoms, but have not yet been confirmed in large clinical studies.
A Generation of Joint Replacements
When diet and exercise modifications, supportive devices, medications and injections no longer sufficiently ease the pain of OA, a hip or knee replacement may be recommended. The number of people opting for this surgery increases each year, now totaling more than 790,000 knee and 450,000 hip replacements annually.
The implants, made of plastic, metal or ceramic, are traditionally kept in place with bone cement, which is gradually being replaced by newer cementless and porous titanium systems to improve bone fixation and durability. Also on the rise is computer-assisted surgery to increase placement accuracy of the prosthetic components, and patient-specific implants using 3D printing technology. The combination of modern materials and advanced surgical techniques have extended the durability of most implants to 20 years, a marked improvement over the previous standard of 10 to 15 years.
Recovery time has also changed for the better. With rehabilitation to regain strength and motion, normal activities can usually be resumed within weeks to months. Most importantly, the majority of patients are highly satisfied with the results, reporting minimal to no pain and significantly improved function and quality of life. However, outcomes can vary and potential complications should be discussed before proceeding.
Additional breakthroughs may be on the horizon: researchers at Duke University start trials this spring of a hydrogel-based cartilage substitute that may prove more durable than natural cartilage…stay tuned!
Every patient is unique…please check with your healthcare provider to discuss recommendations for prevention and treatment based on your individual health situation.
Sources: Arthritis Foundation, AAOS, Orthoworld, Cleveland Clinic, National Academy of Medicine (formerly Institute of Medicine), UpToDate, US Department of Agriculture, American College of Rheumatology.
The post Joint Assets: An Osteoarthritis Update appeared first on Specialdocs Consultants.