Step Up to the Plate: Nutritionists Weigh in on Healthy Eating
Picturing a healthy meal has never been more accessible, thanks to the ubiquity of visual aids such as MyPlate, successor to the well-known Food Pyramid of the ‘90s. A quick scan of the plate’s
quadrants enables users to see at a glance proportions of vegetables, proteins and other foods recommended for a nutritionally balanced day of eating. Hailed as a significant breakthrough when
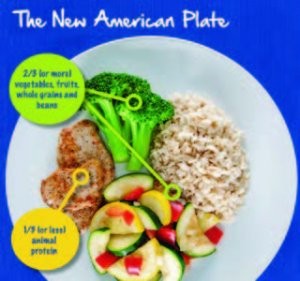
it debuted in 2010, for many dietitians and health experts, MyPlate did not go far enough in revamping the American diet. For instance, Harvard’s Healthy Eating Plate limited red meats but not healthy oils, while the American Institute of Cancer Research’s New American Plate relied even more heavily on vegetables and fruits, accounting for fully two thirds of the plate. The most recent federal guidelines, just issued for 2015-2020, now emphasize shifts needed to choose nutrient-dense foods and beverages in place of less healthy options, and the interconnected relationships between each dietary component. Illustrated at right are what a healthy, and even healthier meal, can look like at your table this year.
MyPlate breaks it down:
- A variety of vegetables from all of the subgroups—dark green, red and orange, legumes (beans and peas), starchy, and other
- Fruits, especially whole fruits
- Grains, at least half of which are whole grains
- Fat-free or low-fat dairy, including milk, yogurt, cheese and/or fortified soy beverages
- A variety of protein foods, including seafood, lean meats and poultry, eggs, legumes (beans and peas), and nuts, seeds and soy products
- Oils
- Limited saturated fats and trans fats, added sugars and sodium (less than 2,300 milligrams per day)
- Alcohol in moderation, up to one drink per day for women and up to two drinks per day for men
- Physical activity: Weekly, strive for 150 minutes of moderate intensity activity (brisk walking) and 75 minutes of vigorous intensity aerobic activity (swimming laps)
The American Institute of Cancer Research (AICR) offers a portion-controlled diet based on fruits, vegetables, whole grains and other plant-based foods that provide an array of cancer-protective compounds while serving as powerful weight-management tool. According to the AICR, the fiber and water in plant foods gives a feeling of satiety with a minimum of calories. Their main message: maintaining a healthy weight is one of the most important steps you can take to reduce your risk of cancer.
The post Step Up to the Plate: Nutritionists Weigh in on Healthy Eating appeared first on Specialdocs Consultants.







